It has only been five decades since scientists began to alter their long-held belief that the human body’s cells, tissues and organs, particularly the heart, strive to maintain a constant static or steady state.
"We now know that the normal resting rhythm of the heart is highly variable rather than being monotonously regular, which was the widespread notion for many years," write the authors of a new article slated to appear in the January issue of Global Advances in Health and Medicine (GAHM), a professional journal.
Variability in heart rhythms, which is gaining scientists' attention around the world today, is the subject of their article, Heart Rate Variability: New Perspectives on the Physiological Mechanisms, and Assessment of Self-Regulatory Capacity and Health Risk. The authors are HeartMath Institute (HMI) Director of Research Rollin McCraty, Ph.D. and Fred Shaffer, Ph.D., BCB of the Center for Applied Psychophysiology, Truman State University, Kirksville, Mo.
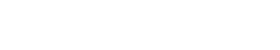
Heart rate variability, the change in the time intervals between adjacent heartbeats, is directly related to the body's interdependent regulatory systems and ultimately, their efficiency and health. "An optimal level of HRV within an organism reflects healthy function and an inherent self-regulatory capacity, adaptability, or resilience," McCraty and Shaffer write.
Although generally the greater the HRV, the better, they note that too much variability, or instability "such as arrhythmias or nervous system chaos is detrimental to efficient physiological functioning and energy utilization… "Too little variation indicates age-related system depletion, chronic stress, pathology, or inadequate functioning in various levels of self-regulatory control systems."
The GAHM article cites much of the pivotal heart rate variability research since 1965, when HRV began to be recognized for its importance in indicating or predicting various risk factors. Among these are fetal distress, autonomic nervous system dysfunction, heart disease, anxiety, depression and asthma among other health conditions.
Many studies, including some conducted by McCraty and others at HMI, correlate an optimal level of HRV, or HRV coherence and coherence training, such as that using HeartMath self-regulation techniques, to a variety of benefits. Among the results of these studies were enhanced cognitive function in a range of age groups and greater functional capacity in heart-congestive patients.
Improvements were demonstrated in a study employing coherence training with a group of middle school students with attention-deficit hyperactivity disorder. Improvements were shown in their short- and long-term memory, ability to focus and behaviors at home and school.
"A study of recently returning soldiers from Iraq who were diagnosed with PTSD," the article states, "found that relatively brief periods of HRV coherence training combined with practicing the (HeartMath) Quick Coherence® Technique resulted in significant improvements in the ability to self-regulate along with significant improvements in a wide range of cognitive functions, which correlated with increased cardiac coherence."
A range of positive health-related outcomes also has been demonstrated in studies with correctional officers who participated in coherence training, McCraty and Shaffer explain. In one study conducted by McCraty, correctional officers improved their blood pressure, total cholesterol and fasting glucose levels and reduced overall stress and fatigue. Similar results were achieved with police officers.
In conclusion, McCraty and Shaffer write, "Numerous studies have provided evidence that coherence training consisting of intentional activation of positive emotions paired with HRV coherence feedback facilitates significant improvements in wellness and well-being indicators in a variety of populations."